 I received an interesting question a couple weeks back from a Cinco Vidas blog reader-is there such a thing as a toxin-free birth control option?
I received an interesting question a couple weeks back from a Cinco Vidas blog reader-is there such a thing as a toxin-free birth control option?
All types of contraception have some risk of toxic exposure, but the risks vary and come from different sources. In the end, the best thing is to review all your options, then make the best choice for your body and your lifestyle.
To help you learn more, below is an overview of today’s most common birth control options, and a note about any related concerns about potential harmful chemicals. Some of the information comes from this great site by Kimberly Snyder, author of The Beauty Detox Solution.
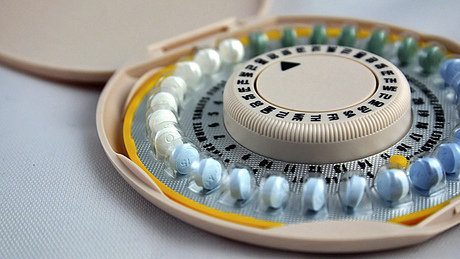
Hormonal Birth Control Pills
The most popular form of contraception, most pills are a combination of estrogen and progestin to help prevent the ovaries from releasing eggs and to decrease the chances of implantation.
High Marks: They’re extremely effective (99 percent), they may reduce your chances of endometrial and ovarian cancer, and some types can actually reduce the number of periods you experience per year.
Low Marks: Long-term use may increase the risk of breast cancer, cervical cancer, and benign liver tumors, though studies are mixed. Newer birth control pills that contain the progestin “drospirenone” (like Yaz and Yasmin) have been linked with blood clots and related complications like pulmonary embolism and stroke. Minor side effects include bleeding, reduced sex drive, mood swings, weight gain, and breast tenderness. Birth control can also increase the risk of melasma, a skin coloration on the face.
Hormonal Patches
These work in a similar way to birth control pills, only the hormones are transmitted through the skin.
High Marks: Same as birth control pills, with an increased convenience.
Low Marks: Same as birth control pills.
Hormone Injections (Birth Control Shot)
This method involves one injection of progestin every three months.
High Marks: Same as birth control pills.
Low Marks: Same as birth control pills, with the added low that you can use this method only for two consecutive years, as prolonged use can result in loss of significant bone mineral density, increasing the risk of osteoporosis.
Vaginal Ring
Also called the “NuvaRing,” this device contains an estrogen and a progestin, similar to birth control pills. Instead of delivering the hormones orally or through the skin, it is inserted into the vagina, where it stays for three weeks. It releases low levels of the hormones into the bloodstream.
High Marks: Same as birth control pills.
Low Marks: Same as birth control pills, with the added side effect of vaginal discharge, that can sometimes occur. Studies with the NuvaRing have also indicated that like Yaz and Yasmin, it may increase risk of blood clots and related complications more than older types of birth control pills.
Implants
A thin rod is inserted in the upper arm that then slowly releases the progestin etonogestrel over a period of three years. (Another brand is designed to last 4 years.)
High Marks: Same as birth control pills, with the added convenience of a three-year solution.
Low Marks: Same as birth control pills, with the added hassle of surgical implantation. Studies show this method is generally well tolerated, though irregular bleeding is a possible side effects.
Male Condoms
The condom is placed over the penis and blocks the semen from reaching the eggs.
High Marks: About 98 percent effective, condoms are easily available, provide protection against sexually transmitted diseases, and involves no hormones.
Low Marks: Most condoms are made from latex, which is highly associated with allergies. When used incorrectly, condoms don’t have as high a protection against pregnancy. To be optimally effective, they should be used with spermicide, which often contains chemicals. The one of most concern is called “nonoxynol-9,” which can cause vaginal and rectal irritation, and may increase the risk of HIV transmission in women. Spermicides also increase the risk of urinary tract infections. There is one so-called “green” spermicide available called “ContraGel Green,” which does not contain nonoxynol-9.
Cervical Cap
A rubber device shaped like a thimble that fits over the cervix, the cap must be inserted 30 minutes prior to intercourse, and must remain in place for 8 hours after ejaculation. A spermicidal gel should also be used.
High Marks: May reduce the risk of Chlamydia or gonorrhea. Uses no hormones.
Low Marks: Has an uncomfortable failure rate of about 7–8 percent. Must be fitted initially by a doctor. The cap can become dislodged during sex, which reduces effectiveness. It can also increase the chance of pre-cancerous changes in the cervix. The spermicide use increases the exposure to chemicals.
Diaphragm
A soft rubber dome, similar to the cervical cap. This device covers the cervix during intercourse. It can be inserted up to six hours prior, and must be left in for six hours afterwards.
High Marks: Easy to use, and uses no hormones. May prevent Chlamydia or gonorrhea infections.
Low Marks: Has a high failure rate (only about 80–85 percent effective). Must be fitted by a doctor. Like the cap, it may become dislodged, which will reduce effectiveness. If it develops holes or tears, this will also reduce effectiveness. Slightly increases the risk of a bladder infection. Requires the use of spermicides.
Female Condom
Called the “Reality vaginal pouch,” this polyurethane sheath with two rings covers the base of the penis and the labia during intercourse. The device is pre-lubricated.
High Marks: Protects against sexually transmitted diseases.
Low Marks: Only 75-80 percent effective. May slip around. Lubrication material may contain chemicals that lead to allergic reactions or irritation.
Intrauterine Device (IUD)
Made of copper or plastic, this device is shaped like a “T” and is inserted into the uterus by a doctor. A thin thread that les against the back of the vagina helps the user determine if the device is still in place. It can remain for several years.
High Marks: Non-hormonal. Copper types are toxic to sperm. IUDs are also highly effective-about 99 percent.
Low Marks: Requires medical insertion, and can increase the risk of pelvic infection, cramping, and heavier periods. The device also slightly increases the risk of ectopic pregnancy (pregnancy outside the uterus).
Hormonal IUD
Similar to the non-hormonal IUD, this device transmits progesterone to prevent sperm from entering the cervix and reaching the egg.
High Marks: Highly effective-about 99 percent. Other benefits similar to birth control pills. Also reduces the risk of tubal pregnancy.
Low Marks: Same as birth control pills and the non-hormonal IUD. Can also cause ovarian cysts and infections.
Sponge
Similar to a diaphragm, the sponge is inserted into the vagina to cover the cervix. Spermicidal foam dried right into the sponge releases when it’s soaked with water.
High Marks: Non-hormonal. May protect from Chlamydia and gonorrhea.
Low Marks: About 85-90 percent effective. May be difficult to remove, and may tear. Can cause irritation, itching, and allergic reactions. May increase the risk of yeast infections. During intercourse, it can become dislodged, reducing effectiveness. The spermicide may contain potentially toxic chemicals.
As you can see, all methods of birth control offer some risk, either of hormonal exposure, chemical exposure, or pregnancy. The only “all-natural” methods are those listed below, but most of these increase the chance for pregnancy. Likely, your needs will change at different stages of your life. Talk the situation over with your doctor to make the best choice for you and your family.
- Cervical Mucus Method: Immediately after your period, levels of cervical mucus decrease, then later return as the body prepares for ovulation. Tracking the mucus pattern can help you determine your “safe” days (dry days).
- Calendar Method: Ovulation occurs 14 days prior to menstruation. An egg can be fertilized for 24 hours afterwards, and a sperm can live for 48–72 hours after ejaculation. In this method, a woman tracks her periods for six months-the unsafe period is calculated by subtracting 18 from the shortest cycle to get the first fertile day, and 11 from the longest cycle to get the last fertile day. This method works only for those women with very regular periods. (See more here.)
- Temperature Method: Body temperature drops slightly before ovulation, and rises after. A woman charts her temperature changes by recording it first thing in the morning for several months, then determines her safe days. This method is usually combined with the other two.
What do you think is the safest, most non-toxic method of birth control for you? Please share your thoughts.
Picture courtesy theseoduke via Flickr.com.

